Lessons Learned from the Indigenous Birth Support Worker Program
One year after the implementation of the Indigenous Birth Support Worker (IBSW) Program, a study was conducted by the Saskatchewan Health Authority (SHA) Research Department in collaboration with Maternal Services at the Jim Pattison Children’s Hospital (JPCH) to examine and document the lessons learned.
The IBSW program was developed to provide Indigenous women culturally-responsive care and support during labor and birth and postpartum. Located in Jim Pattison Children Hospital in Saskatoon, the program was created as part of the response to a 2017 report detailing the experiences of many Indigenous women regarding tubal ligation procedures. It also aligns with Truth and Reconciliation Calls to Action number 22.
IBSWs received training that was coordinated in collaboration with SHA and Gabriel Dumont Technical Institute. The training consisted of:
- knowledge about traditional birthing practices
- doula training that was delivered based on the educational standards outlined by DONA International. IBSWs also received additional orientation from the Maternal Services unit. The program was implemented in December 2019. Out of the 1023 clients who registered for the program between December 2019-January 2021, 56% were from out-of-town.
Interviews with clients indicated they greatly appreciated the cultural support and compassionate, non-judgmental, and safe care provided by the IBSWs.
“I found them [IBSWs] really supportive, received a moss bag, beaded earrings. I came to the hospital in shorts and I didn’t have anything. They brought me shoes, shampoo. I came to the hospital alone so it was nice to have them. They were really supportive, friendly and made me feel comfortable. It was great that IBSW took me upstairs (NICU) to see my baby right after delivery. She didn’t have to but she did. I enjoyed my time with them.”
The cultural support and traditional wisdom provided through the IBSW program were well received by clients and families.
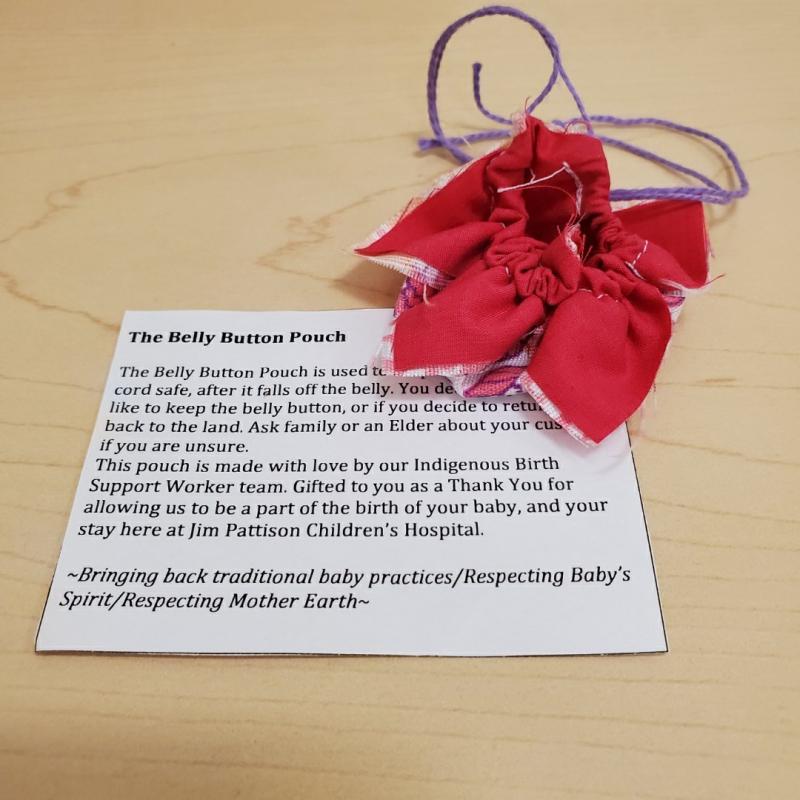
“I like that she’s thorough. She really makes sure that we have the information we need. I like that she gave us pamphlets on the different teachings, traditional teachings, and the little belly button pouch. And it was comforting to know those were offered services here at the hospital, ‘cause I just felt like it represented us as a family and what we would want in our baby’s care.”
In a focus group carried out with IBSWs, they emphasized the need for culturally safe and client-centered care, which includes other family members.
“I’ve had dads ask, “Can you teach me how to do the moss bag?” I always ask, I always try to include the men, too. And if it’s a sister or Kookum involved, having them incorporate stuff. And usually, they already know, so they’re already doing this stuff. It’s really nice when you see that.”
IBSWs indicated the need to develop relationships with community elders and healthcare teams to ensure there is smooth hand over of care to and from the communities to the urban care centre.
“If we integrate with the community, and their Elders, and their ways of knowing…and kind of just build that relationship so we can call upon them. So when a member of their region comes into our space, we can have that communication, and having just that relationship with the community, I feel like would really benefit the women. So they don’t feel like they’re in a foreign place, completely away from their people.”
Survey results from healthcare providers indicate they were interested in learning about Indigenous birthing strategies: there was a strong consensus to integrate Indigenous birth practices with Western best practices for clients who prefer it.
Suggestions to improve and expand the current program include:
- increased access to Elders and spiritual care, traditional teachings during pregnancy, childbirth, and perinatal loss
- a stronger partnership between IBSWs and mainstream healthcare providers
- employ the study results to plan allocation of resources and staffing for the next year and inform scale-up plans
- scale the program to other locations.
A final report and publication will be published in the coming months.
For more information about this research project, please contact Dr. Mamata Pandey, Research Scientist, SHA Research at mamata.pandey@saskhealthauthority.ca. More information on the program in general is available on the SHA website.