Opioid Use Disorder
What is opioid use disorder?
Opioid use disorder is characterized by the ongoing use of opioids despite harmful consequences that can significantly affect your health and/or function at work, home, or school.
There is a common misconception that opioid use disorder (sometimes called opioid addiction) is a choice and that people can stop using opioids when they want to. Opioid use disorder is a treatable chronic disease, not a choice.
Anyone can develop an opioid use disorder. In episode 2 of an audio series on opioids developed by Health Canada, a physician tells his story of developing an opioid use disorder during treatment of his back pain.
Management of opioid use disorder
Management for opioid use disorder combines the use of medication (opioid agonist therapy) with non-pharmacological therapies e.g., counseling, cognitive behavioural therapies, traditional ceremonies and culture.
Opioid agonist therapy may include one of the following medications:
- Buprenorphine-Naloxone (Suboxone®)
- Methadone (Methadol®)
- Long Acting Morphine (Kadian®)
Risk of opioid overdose
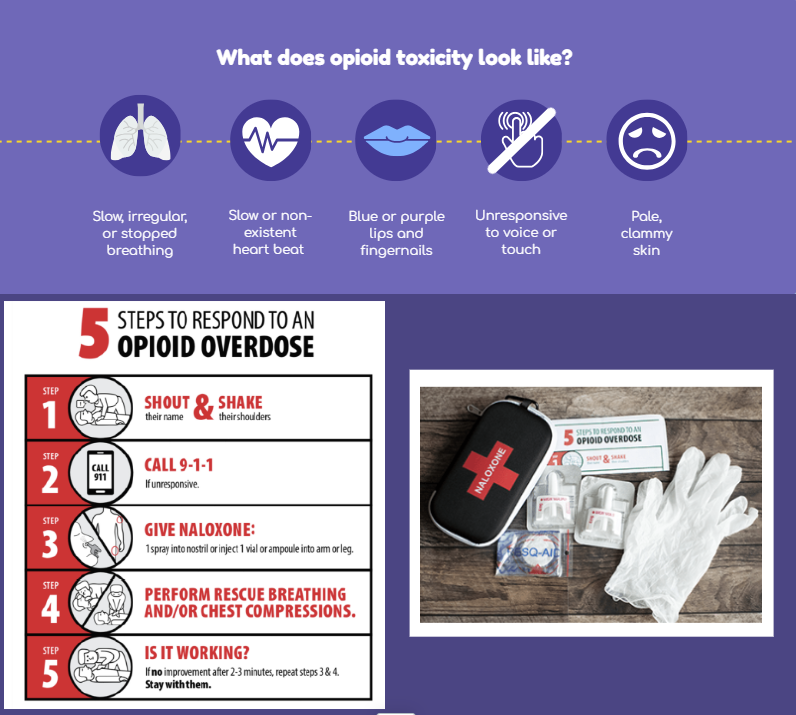
The number one risk associated with opioid use disorder is opioid overdose, also known as opioid toxicity or poisoning. Opioid overdoses can be fatal. Know the signs of opioid overdose. Ask your healthcare team about Take-Home Naloxone Kits if you or someone you know are at risk of an opioid overdose. You can get a free Naloxone kit from Take-Home Naloxone Program Sites OR buy (without prescription) from some pharmacies.
Concurrent Disorders
What is a concurrent disorder?
Concurrent Disorders refers to two primary conditions that occur simultaneously in an individual. The conditions are mental health and substance use disorder. The definition has expanded to include those that may have psychiatric symptoms. This condition is also known by several other terms, including:
- Co-occurring disorders
-
Comorbidity
-
Dual disorders
-
Dual diagnosis
These disorders can involve any combination of mental illnesses/ disorders such as anxiety, depression, schizophrenia, etc, and substance use issues such as alcohol, drugs, gambling, etc. It is not uncommon for individuals to use multiple substances and have more than one mental health disorder/diagnosis.
Individuals can also have conditions induced by substance use like anxiety, mood or psychotic symptoms; although not technically a concurrent disorder, the reality of care is that some clients will demonstrate substance induced conditions that may convert to disorders.
Prevalence
Research shows that more than 50% of those seeking help for substance use disorder also have mental illness, and 15-20% of those seeking help from mental health services are also living with a substance use disorder. It is important to note the depending on the disorder the prevalence rate of concurrent disorder may be higher or lower.
Why Does It Happen? There are several reasons why concurrent disorders develop, such as:
-
The presence of a mental health condition may lead to an substance use disorder, or vice versa (known as the direct causal hypothesis).
-
One condition has an effect upon an intermediary factor that, in turn, increase the likelihood of developing the second condition (known as an indirect causal relationship).
-
Two conditions may also come about due to the presence of shared biological, psychological, social, or environmental risk factors. That is, the factors the increase the risk of one condition may also increase the risk for another (known as common factors).
What Comes First? Sometimes the question of what came first, the mental health or substance use disorder comes up. This question can lead to the perception that if one disorder is treated i.e., the one that came first such as a mental health disorder, the individual will have less of a need to use substances. This is a false narrative. In only a few cases does a mental health disorder clearly lead to the development of a substance use disorder. An example would be someone with long-standing major depressive disorder who starts using alcohol excessively to cope and then develops a substance use disorder. Another example where substance use clearly precipitated a mental disorder would be if someone develops a cocaine-induced psychotic disorder. In many cases, it will be uncertain which disorder occurred first. In addition, there may be a third condition that is influencing both or either of the two comorbid disorders (e.g., HIV, chronic pain). Environmental factors, like homelessness or extreme stress, can also affect one or both disorders. Thus, even when it is clear which disorder developed first, the causal relationship may be unknown. The nature of concurrent disorders is inconsistent and nuanced. This means that both need to be treated with equal seriousness. Once both disorders are evident, they both need to be treated as one condition as one may exacerbate the other, interact with the other, and overall impact the other - the relationship between them is considered bidirectional.
How To Treat?
There can be the belief that clients who have both substance use and mental health disorders are self-medicating symptoms of either disorder and typically the belief is related to the idea that using substances is a means of coping with mental health symptoms. Although some people with mental conditions may misuse substances to alleviate their symptoms or otherwise cope, this is not always the case. Once both disorders are evident, they both become primary and need to be treated. Unfortunately treating one condition has not been demonstrated to “fix” or “heal” the other. This can also include concurring trauma and substance use disorder, anxiety and substance use disorder, mood disorders and all other combinations.
Because of the complexity and interrelated nature of these issues, individuals with concurrent disorders tend to face more significant challenges than those with just one of the conditions. Individuals with concurrent disorders are more at risk for negative outcomes such as:
To achieve the best outcomes, it's crucial that both mental health and substance use issues are addressed simultaneously and in a coordinated manner (integrated treatment). This integrated care approach leads to more responsive and effective support, helping individuals manage both aspects of their condition.