Information for Healthcare Professionals - Tissue and Organ Donation
Organ Donation
Organ donation plays a crucial role within end of life care options for the people of Saskatchewan. Hospitals, equipped with medical technology and expertise, often manage complex cases involving severe trauma, critical illnesses, and handling end-of-life care.
When a patient experiences an irreversible loss of brain function or traumatic injury/illness, and all resuscitative efforts have been exhausted, the hospital's dedicated organ donation team, in collaboration with the medical staff, carefully assesses the potential for organ donation. This process involves a thorough evaluation of the patient's present medical conditions, medical history, the cause of death, and the health of their organs. If deemed suitable for donation, and the family is agreeable to donation, the team works diligently with the medical staff to preserve organ function while coordinating the retrieval and transportation of organs to transplant recipients in need across the country. Tertiary hospitals serve as vital hubs for organ donation, offering hope and a second chance at life for countless individuals awaiting transplantation.
Organ donation opportunities may arise following catastrophic traumatic events or accidents. After all resuscitative efforts have been exhausted and brain death has been and there is no meaningful recovery, the potential for organ donation may be identified. Catastrophic traumatic events or accidents that may lead to an organ donation path may be:
- Severe Traumatic Brain Injury (TBI): This can include injuries from car accidents, falls, assaults, or strokes. If the brain injury is severe enough, it can lead to brain death.
- Anoxic Brain Injury: This occurs when the brain is deprived of oxygen for an extended period, such as during prolonged cardiac arrest or drowning.
- Severe infection: Meningitis can cause significant damage to the brain. Even with a severe infection organ donation can still proceed.
- MAiD: Those that are considering MAiD due to their condition, can potentially be a organ donor. Currently this can only be brought up once patient has been fully accepted into MAiD, and needs to be patient led. (ie: Client must ask to speak with Organ Donation team) MAiD Program
It is important to remember that even individuals who have a catastrophic injury that falls under the jurisdiction of a coroner, they can still be considered for organ donation. Coroner cases, such as accidental deaths, attempted suicides, or attempted homicides, do not automatically disqualify someone from being considered for organ donation. The Coroner will carefully assess the circumstances of the death to determine if organ donation is medically possible and ethically appropriate.
Brain-based definition of death
Please see this educational video
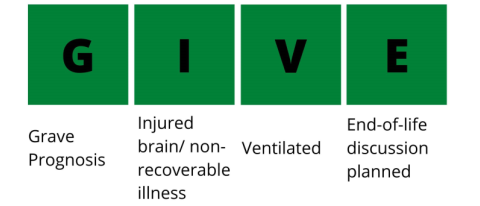
A member of the health care team will notify the Donor Coordinators for all individuals who meets GIVE criteria. Donor Coordinators will assess the referral for organ donation eligibility.
- G - grave prognosis or Low GCS
- I - injured brain/non-recoverable injury/illness
- V - ventilated
- E - end of life discussion planned, but prior to WLSM
It is important to remember any hospital with the ability to determine catastrophic injury to the brain, those with imaging. Are able to refer to the donation team for organ donation. If a potential donor had their accident outside of the tertiary hospitals, we are able to transfer them to Regina or Saskatoon if the next of kin or family agree to organ donation. The MRP would have to determine that there is a non recoverable injury/illness, supported with imaging, consult specialist in Regina or Saskatoon to see if there is any treatment options for the patient. If the specialist states there is nothing that can be done, the patient now meets GIVE, and a referral can occur. We can transfer to Regina or Saskatoon for the sole purpose of organ donation. All residents of Saskatchewan have the right to choose if donation is right for them or their loved ones. As healthcare workers, we can lead the conversation, and offer information to ensure they can make the best decision for them.
How Organ Donation Works educational video
Death by Neurological Criteria (DNC)
Neurologically determined death is defined as the “irreversible loss of the capacity for consciousness combined with the irreversible loss of all brainstem functions, including the capacity to breathe” (Canadian Neuro-critical Care Group 1999). Previously, the terms “brain death”, “neurological death” and “death by neurological criteria” were used interchangeably.
Diagnosing neurological death involves determining the irreversible loss of brain stem reflexes, such as cough, gag, corneal, vestibulo-ocular and pupillary response to light. These must be tested without any confounders present, such as sedating medications, abnormal electrolytes or acid base balance. They must also have an injury that can lead to neurological death, this must be supported with medical imaging that shows injury to the brain. There can be no spontaneous movement or central response to pain, although spinal reflexes may persist. The person is also no longer able to breathe (apneic), requires mechanical ventilation and their capacity for consciousness has been irreversibly lost. Neurological Death does not need to be determined prior to offering Donation.
What are some conditions may lead to neurological death?
- Acute brain injury: Head trauma from motor vehicle collisions, intracranial hemorrhage from any cause including stroke, intracranial tumor or acute hydrocephalus.
- Hypoxic-ischemic encephalopathy: Post-cardiac or respiratory arrest, near drowning, asphyxia, hypovolemic shock.
- Central nervous system (CNS) infection: Meningitis, encephalitis, generalized sepsis.
- Miscellaneous: Metabolic encephalopathy from liver disease; diabetic ketoacidosis, metabolic disorders, acute hyponatremia or vasculitis.
Death Determination by Neurologic Criteria (DNC), formerly NDD, is primarily a clinical assessment that requires all three of the following:
- Absence of consciousness (lack of wakefulness and awareness in response to stimuli);
- Absence of brainstem function (cranial nerve testing) and;
- Absence of the capacity to breathe (formal apnea testing)
Prior to conducting any part of the clinical assessment for DNC, the following prerequisites must be met:
There must be an established cause of devastating brain injury severe enough to cause death and is supported by neuroimaging evidence; AND
Potential confounders of an accurate clinical assessment must have been considered and excluded *see reverse of the Death Determination by Neurologic Criteria (DNC) Checklist
Clinical Assessment: Must be completed by two staff physicians and documented on the Death Determination by Neurologic Criteria (DNC) Checklist. Both staff physicians may conduct the full clinical assessment concurrently. If completed at separate times, each staff physician must complete all components of the clinical exam. The exam is to determine the absence of cranial nerves. This exam must be carried out by physicians who are well versed in critical care and determining brain death.
The clinical assessment also tests for the absence of spontaneous breathing. This component is known as apnea testing and it is recommended that this be the final component of the clinical assessment.
If any portion of the clinical assessment, including apnea testing, cannot be completed and/or potential confounders cannot be excluded, ancillary investigation is required. Ancillary testing is also required for any isolated infratentorial brain injury without supratentorial involvement.
Death by Circulatory Determination (DCC)
In Saskatchewan, organ and tissue donation after death by circulatory determination (DCC) is a possibility for patients who do not meet the strict criteria for neurological or brain death but still suffer from a non-recoverable injury. Patients who meet the criteria for DCC are dependent on mechanical ventilation. DCC is a possibility for families who have decided to withdraw life sustaining therapy after a physician has determined that there is no recovery. This may include patients at end-of-life with chronic ventilator-dependent conditions (i.e. Amyotrophic Lateral Sclerosis, Muscular Dystrophy etc.). If the end of life conversation and withdrawal of life support is planned to occur outside of Saskatoon or Regina, and the family is interested in donation, we are able to arrange for transport to one of our ICU’s to fulfil the families’ wishes; but withdrawal of life sustaining therapies cannot have started prior to transfer.
This is the path that a MAiD client would qualify for. MAiD would need to happen at a hospital in either Regina or Saskatoon. Timeline is explained to the potential donor and their family. They may need to come to the hospital or lab in advance for testing prior to allocation.
When it comes to the act of donation, unlike DNC, DCC that patient will be extubated and all infusions will be stopped. Compassionate infusions would continue. Typically the withdrawal of life sustaining therapies will cause the patients blood pressure to drop, which causes a lack of perfusion and oxygenation to the organs. This can cause damage to them. Because of this, there is a time limit in which the patient would have to pass away within, in order to proceed with organ donation.
Ocular Donation
Ocular donation is a truly remarkable gift that can profoundly impact the lives of individuals suffering from vision loss. In Saskatchewan, ocular donation involves the cornea and sclera. The cornea, the clear, dome-shaped front surface of the eye, it is responsible for focusing light, roughly 70%, onto the retina, which allows people to see. When damaged or diseased, the cornea can significantly impair vision, leading to blurred or distorted sight, severe pain, and even blindness. Corneal transplants, a relatively highly successful surgical procedure, involve replacing the damaged cornea with healthy donor tissue. This life-altering procedure can restore sight to individuals suffering from conditions such as:
- Keratoconus: A progressive eye disease that causes the cornea to thin and bulge outward, distorting vision.
- Corneal scarring: Resulting from infections, injuries, or previous eye surgeries.
- Fuch's endothelial dystrophy: A hereditary degenerative condition that affects the inner layer of the cornea, causing it to swell and impair vision.
The impact of a successful corneal transplant is immeasurable. It can allow individuals to regain independence, return to work or school, and simply enjoy the everyday pleasures of sight, such as reading, driving, and appreciating the beauty of the world around them.
Scleral donation is another part of ocular donation. The scleral tissue is used for a multitude of sight save/eye saving surgeries, cosmetic procedures and can be used for glaucoma shunt surgeries.
Moreover, ocular donation is a selfless act that offers hope and a renewed sense of purpose to those facing vision loss or the threat of vision loss.
The Ocular Donor Assessment Form (found below) is completed on every death in the SHA. This completed form is sent via Email or Fax to the SHA Donation Program found at the bottom of the referral form. The goal is to ensure all patients and their families have the opportunity to make an informed decision regarding ocular donation.
- The Ocular Donor Donation Assessment Form highlights deferral criteria for tissue donation.
- If the answers to all questions on the form are NO please call the SDP Coordinator on call through hospital switchboard. If there are any YES’ ticked on the form, fax/email the completed form; but you do not need make a phone call.
- Ideally a call is made within one hour after someone has passed.
Consent for ocular donation can occur prior to death or after death. When death is anticipated families or next of kin (NOK), can provide consent for ocular donation prior to the death of the individual. When death is imminent it is acceptable for the individuals to provide first person consent, this can happen with any palliative patients. The form can be filled out prior to passing and sent into the program. A coordinator will review and call the unit to discuss the possibility of donation. Palliative and MAiD patients are in unique circumstances to have the consent done before passing. The act of donation will only happen after passing.