Treatment Choices for Kidney Failure
It is essential to know all about what treatment choices are available to you when/if your kidneys stop working.
There are three main treatment choices:
- Dialysis
- Kidney transplant
- Conservative kidney management
Think about what is important to you and your family when making decisions. Sometimes it is hard to think about these things. When making decisions, people often consider the following:
- What is my prognosis? You will need to ask your kidney doctor about this.
- How important is leading an active life or maintaining my independence to me?
- What are the diet and fluid restrictions like for this treatment choice?
- Can I travel for fun?
- Can I continue to work or go to school?
- What is my home situation like?
- Do I look after others – children, parents, or others?
- What are the side effects of the treatments or drugs that are needed?
- What will my quality of life be like?
- How far will I have to travel for appointments or treatments?
- Anything else of importance to you.
Sometimes decision aides can guide your thoughts and help you organize your questions for your kidney care team. The following resources may be helpful:
- A decision aid for the treatment of kidney disease.pdf
- Living With Kidney Failure: Chapter 1 - Exploring Treatment Options
It is important to plan ahead. The better you are prepared for what is ahead of you, the better your health will be. No matter what treatment choice you choose, everyone should take part in advance care planning (ACP). ACP is a process in which you think about what you would like to happen or not happen if you become unable to make decisions or communicate about your healthcare wishes
1.Dialysis
There are two types of dialysis
- Peritoneal dialysis
- Hemodialysis
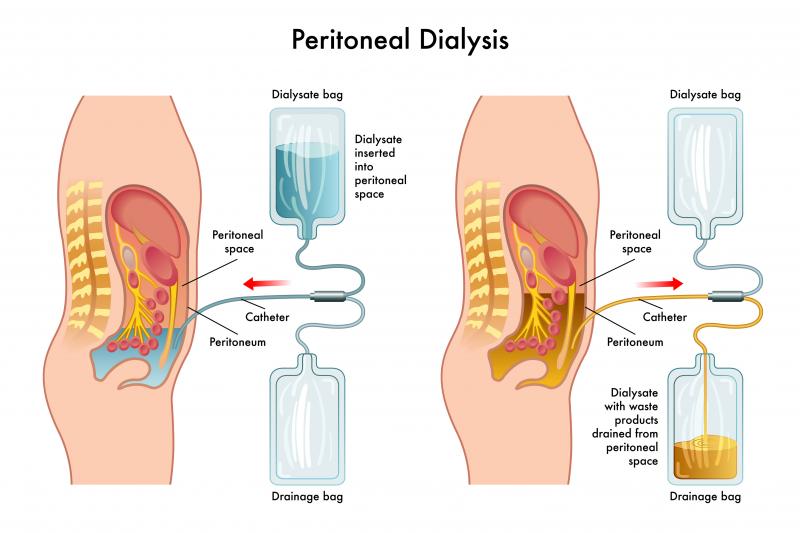
Peritoneal Dialysis – often called PD
- Uses the peritoneum to clean the blood.
- The peritoneum is the membrane which lines the abdominal cavity and covers the abdominal organs. It provides the passage for small blood vessels and lymph to travel to and from the abdominal organs. Between the peritoneum that lines the abdominal cavity and the peritoneum that lines the organs (like the small and large intestines) is the peritoneal cavity.
- A tube, called the peritoneal dialysis catheter, is inserted into the peritoneal cavity (in the operating room, in the X-ray department or at the bedside) and is used for peritoneal dialysis.
- A special type of sugar based fluid is put into the peritoneal cavity and the toxins, waste products and excess water flow into the solution in the peritoneal cavity through the small blood vessels. After about 4 to 6 hours this fluid is drained, and a new bag of fluid is put into the peritoneal cavity and the cycle is repeated. This process is called continuous ambulatory peritoneal dialysis or CAPD. Usually, about 4 cycles per day need to be done.
- Peritoneal dialysis can also be done by a machine that is attached to the peritoneal dialysis catheter. This process is called automated peritoneal dialysis or APD and is done at night while you sleep.
- Peritoneal dialysis must be done every day.
- Some of the benefits of PD are:
- You can do it at home.
- Your dialysis is flexible so you can fit it around your life.
- It is easy to take your PD with you when you travel or go to the cottage.
- There is less stress on your body as PD is more like your natural kidney function.
- Your diet may be less restrictive.
- There are no needles with PD.
- PD helps preserve what remaining kidney function you have.
- You can do PD while you sleep.
- Some of the drawbacks are:
- You will need a catheter in your body.
- You will not be able to have baths, sit in a hot tub or swim in a lake because of the risk of infection.
- PD needs to be done daily.
- There is a small risk of infection.
- There may be some weight gain because of the sugar-based PD fluid.
Hemodialysis – often called HD
- Uses a machine to clean the blood.
- Blood is taken from the body through a arteriovenous fistula (AVF) – a connection between the artery and vein in your forearm or upper arm, or arteriovenous graft (AVG) – a connection with a plastic tube between the artery and vein near your elbow or by a large intravenous tube (central venous line or CVL) in the big vein of your neck (internal jugular vein). The blood is taken from your body by a HD machine and passed through a dialyzer – artificial kidney where the toxins, waste products and excess water are removed. The clean blood is cycled back into your body. Usually, all of your blood is exchanged about 5 times during a HD treatment.
- HD is typically done 3 times per week for about 4 hours each time.
- HD can be done at home, in a hospital, satellite unit or free-standing clinic.
- HD can be done independently in your home or in a self-care clinic. There is always support available to you.
- Some benefits of independent HD include:
- Your HD schedule fits around your life, job, or school.
- HD can be done at night while you sleep.
- Generally home HD allows you to do more dialysis and therefore results in better health, and more energy.
- Fewer medications and less restrictive diet.
- Some drawbacks of independent HD include:
- You will need access to specialized electrical and plumbing. Your home many need some renovations – dialysis programs generally pay for one-time renovations.
- You will need storage space for supplies.
- Needles are generally required.
- There is a 6 to 8-week training period.
- Some benefits of independent HD include:
- Dependent HD is done in a hospital. satellite unit or free-standing clinic
- Some benefits of dependent HD include:
- 3 to 4 times per week, 4 to 5 hours each time
- You can socialize with other patients.
- There is no equipment or supplies in your home.
- Kidney health team members manage your care.
- Some drawbacks of dependent HD include:
- There is very little flexibility in your schedule.
- It is harder to travel.
- Usually, you will spend more than 4 to 5 hours in the hospital waiting to get on and off the HD machine.
- You may have parking and transportation costs and will have to travel to the HD clinic 3 to 4 times per week.
- Your diet and fluid intake are more restrictive.
- Needles are generally required.
- Some benefits of dependent HD include:
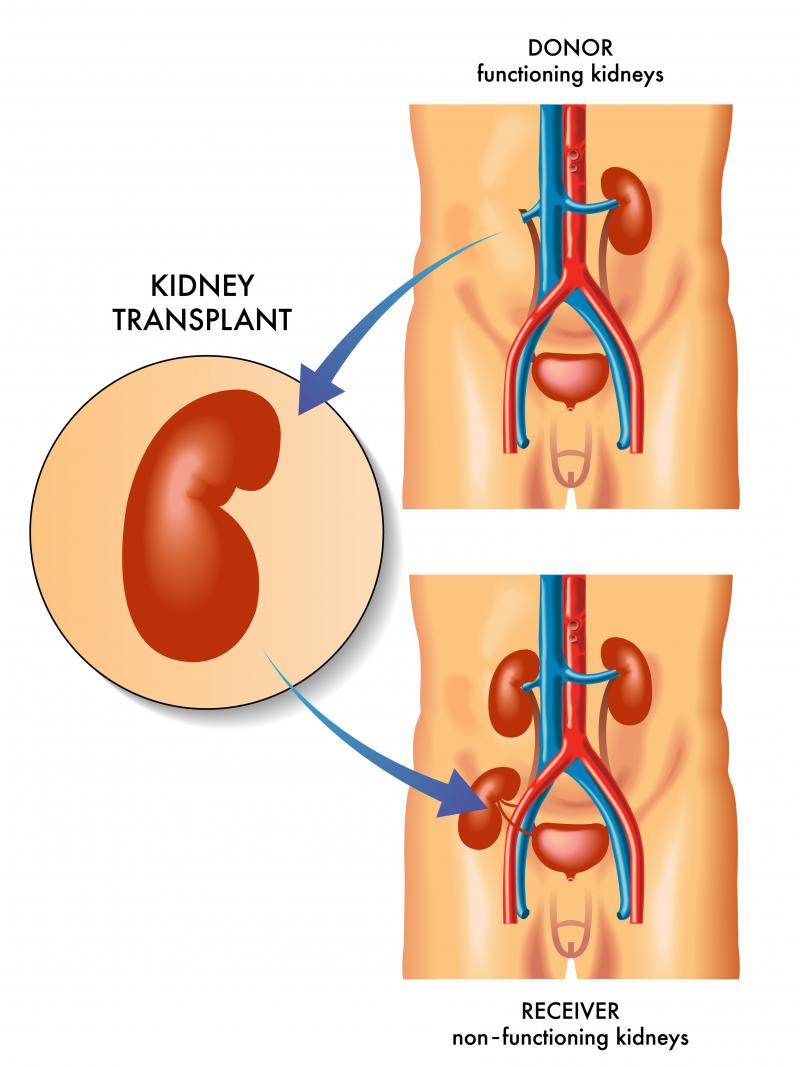
2. Kidney Transplant
- The best choice for treatment when kidneys fail is a kidney transplant, if possible.
- Kidney transplant is a treatment NOT a cure.
- Why is a kidney transplant the best treatment?
- There is a significantly reduced risk of death in comparison to dialysis treatment.
- You will live longer.
- There is a reduced risk of heart attack, stroke, and heart failure.
- There is less chance of being hospitalized for an infection.
- Your quality of life will be better.
- You are more likely to continue to work.
- However, as with anything, there are risks of kidney transplant.
- Your body may reject the kidney – although this happens less now with newer medications.
- The kidney may not work – this is called acute kidney rejection.
- Risk of infections and some cancers, such as skin cancer, are higher because you have to take anti-rejection medication.
- Risk of diabetes, high blood pressure and high cholesterol is higher.
- Some of the anti-rejection drugs can cause long term kidney damage. They are used however because at present they are very good at preventing rejection.
- There are three types of kidney donors:
- Living related
- Living non-related
- Deceased
- A living donor is best because the transplant can be scheduled at a time convenient to the donor and the person getting the transplant. Living donor transplants also last longer in most people than deceased donor transplants. Living donors have an extensive work-up to ensure they are healthy and able to donate one of their kidneys.
- Overall, in people who can have a kidney transplant the benefits definitely outweigh the risks.
- Who is suitable for a kidney transplant? People who are suitable should have:
- Irreversible kidney disease – sometimes people have acute kidney failure which gets better over time. These people do not need a kidney transplant.
- Because of the anti-rejection medications, people cannot have active cancer or infection as the anti-rejection medications will make the cancer grow more rapidly and the infection could be life threatening. If you have had previous cancer, there is a waiting period for you to be cancer free before you could have a kidney transplant. This waiting period depends on the type of cancer you had.
- A good transplant candidate must be able to withstand the surgery and have a life expectancy of more than 5 years.
- The transplant journey can be a difficult one, so family and social supports are especially important to help you along.
- You must be able to take your medications faithfully and follow-up with all appointments and instructions from the Transplant team. Having a kidney transplant is a gift that needs to be taken of.
- The people not suitable for a kidney transplant are those with:
- Active cancer
- Moderate to severe lung or heart disease
- Severe blood vessel disease in the pelvis and leg vessels – because the surgeon will not be able to attach the kidney artery and vein if the blood vessels are too hard and stiff.
- Cirrhosis and not a candidate for a liver transplant.
- Dementia - some of the anti-rejection drugs make this worse.
- Active drug or alcohol addiction including smoking tobacco and marijuana as this makes taking other medicines difficult. People need to have attended addiction counselling and be drug and alcohol free for at least 6 months before a transplant can be considered.
- If you have problems taking your medicines before transplant, you may not be considered a transplant candidate.
- The person who is having the kidney transplant – called kidney recipient will have an extensive workup to ensure that they can have the surgery.
3. Conservative Kidney Management (CKM)
- Conservative kidney management may be a better treatment option for some people as it focuses on quality of life, symptom management and living well without dialysis.
- Why would you choose conservative kidney management?
- Dialysis may not help everyone live longer or improve their quality of life.
- For some people, the side effects of dialysis may even lower their quality of life or make them feel worse.
- Dialysis does not treat other medical problems like diabetes, heart problems, arthritis, or pain.
- Other reasons to choose conservative kidney management include:
- Some people feel the burden of dialysis is not worth the benefits of dialysis and so opt for conservative kidney management.
- Some people will not do well on dialysis which means they will not live longer or feel better. These people often have other serious illness such as heart disease, some types of cancer and dementia. People who are already very frail – needing help with basic activities of daily living like bathing, getting dressed or walking even with an aide – often do poorly on dialysis and decline quickly to the point they need nursing home care.
- What should you consider when making your decision about conservative kidney management? Things to think about include:
- What is your prognosis? If you do not know, ask your kidney doctor.
- How important is leading an active life, being independent to you.
- What are your other medical conditions?
- What are the side effects of dialysis treatments? Will I be able to tolerate these?
- What will my quality of life be on dialysis?
- People who are older than age 80 generally do not do well on dialysis. They have more complications from dialysis and the risk of death is higher.
- Anything else of importance to you?
- What do you need to consider in order to make your decision about conservative kidney management?
- There is a helpful patient decision aide at www.ckmcare.com
- This tool considers such things as your values and beliefs, where you are living, your age, your current health, and activities.
- This tool focuses on quality of life, prognosis, treatment choices and chances of survival.